The total number of COVID-19 cases in on the rise, and so is the death toll. In the context of the coronavirus pandemic, it is normal to feel overwhelmed by all the negative information. But researchers are trying their best to understand, treat, and prevent the new coronavirus.
As of yesterday, the total number of deaths caused by COVID-19 across the world has surpassed 34,000, while the total number of confirmed cases around the globe stands at 724,000.
It’s true that everything is so scary and these numbers can induce restlessness and worry, and the importance of taking precautions and staying safe during this global pandemic shouldn’t be overestimated. However, it is also helpful to take a look at some emerging research that could pave the way for future treatment and prevention.
Infection control measures work
Researchers in Hong Kong have analyzed the effect that the coronavirus outbreak has had on 43 public hospitals there.
Additionally, the numbers are encouraging: In the first 6 weeks since the start of the coronavirus outbreak, 413 healthcare workers dealt with 42 confirmed cases of COVID-19. Of these 413 employees, 11 had unprotected exposure to the new coronavirus.
However, as a result of implementing the best practices for infection control, none of the healthcare staff contracted the virus during the study period. Furthermore, no hospital-acquired infections occurred.
Dr. Vincent C.C. Cheng, from the Department of Microbiology at Queen Mary Hospital in Hong Kong, and his colleagues conclude:
“Appropriate hospital infection control measures can prevent healthcare-associated transmission of the new coronavirus Vigilance in hand hygiene practice, wearing of surgical masks in the hospital, and appropriate use of personal protective equipment in patient care are the key infection control measures to prevent hospital transmission of the virus.”
Getting the virus may protect against reinfections
A new study found that contracting SARS-CoV-2, the virus that causes COVID-19, protected against future reinfections.
The scientists reinfected two of the four monkeys with the virus 28 days after the initial infection to find out more related information about this virus.
A total of “96 nasopharyngeal and anal swabs tested negative after the reexposure of SARS-CoV-2,” report the researchers. Moreover, these results were confirmed by the euthanasia and necropsy of one of the two monkeys.
“Taken together, our results indicated that the primary SARS-CoV-2 infection could protect from subsequent exposures, which have vital implications for vaccine design and disease prognosis,” conclude the authors of the study.
“I can tell you, if you got [COVID-19] and you got really sick, I am sure that will make an antibody response that will also last,” explains Martin Bachmann, a professor of vaccinology at Oxford University’s Jenner Institute in the United Kingdom, on the broader subject of COVID-19 and building up immunity to the virus.
Prof. Bachmann, who is also the head of the department of immunology at the University of Bern in Switzerland, continued: “But, if you have the virus and it only replicates a little and never really reaches the lymph nodes, then maybe you don’t really make [an antibody response], but then you have not really been sick. Of anyone who has been really sick, I would be surprised to find anyone who didn’t make an antibody response.”
A vaccine is being trialed, more underway
At the moment, a trial is currently taking place to test a potential SARS-CoV-2 vaccine for the first time in humans.
The National Institutes of Health (NIH) have funded the trial, which is taking place at the Kaiser Permanente Washington Health Research Institute in Seattle.
Furthermore, 45 healthy volunteers agreed to receive a vaccine that contains a part of genetic code copied from SARS-CoV-2. Also, it’s important to know that the vaccine does not contain the actual SARS-CoV-2, so the participants will not develop COVID-19.
However, the Government officials explain that it may take up to 12–18 months before the vaccine can reach the market. They also explain that the main purpose of this current trial is to make sure that there are no serious side effects.
However, a research editor, Yella Hewings-Martin, Ph.D., rounded up several projects that identified a potential vaccine and therapy targets for SARS-CoV-2.
An old method could fight COVID-19
Doctors may be able to use an old method called “passive antibody therapy” to treat COVID-19, suggests research featured in The Journal of Clinical Investigation.
The researchers who authored the paper say, “Deployment of this option requires no research or development,” as the method has been around since the 1930s.
The method consists of collecting blood from a person who has had the virus and recovered from it. The part of the blood that contains infection-fighting antibodies has to be injected in another person, and it will either prevent infection or help to fight it off.
Dr. Arturo Casadevall, a professor at Johns Hopkins Bloomberg School of Public Health in Baltimore, MD, and co-author of the new paper, says:
“It’s all doable — but to get it done, it requires effort, organization, resources… and people who have recovered from the disease who can donate the blood.”
Our immune system could defeat the virus
Another recent study, appearing in the journal Nature Medicine, documents the case of a COVID-19 patient who recovered from the condition within days.
The researchers examined the immune response of the patient because they want to understand her recovery, it’s the case of a 47-year-old woman who had contracted the virus in Wuhan, China.
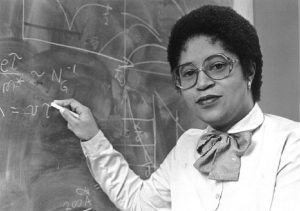
Prof. Katherine Kedzierska, Head of the Human T cell Laboratory in the Department of Microbiology and Immunology at the Doherty Institute in Melbourne, Australia, and her colleagues found an increase in immunoglobulin G in the woman’s blood samples, which is the most common type of antibody. Additionally, they also found an increase in immunoglobulin M.
The scientists also found a high number of key immune cells, such as specialized helper T cells, killer T cells, and B cells, 7–9 days after symptom onset.
“This is an incredible step forward in understanding what drives recovery of COVID-19. People can use our methods to understand the immune responses in larger COVID-19 cohorts and also understand what’s lacking in those who have fatal outcomes.” – Prof. Katherine Kedzierska