Men appear to produce higher levels of COVID-19 antibodies than women, according to statistics. Covid-19 survivors are being asked to donate blood plasma as part of a major study assessing whether it might help some of the sickest patients. The study is ongoing to evaluate whether convalescent plasma donations can be transferred to patients struggling to develop their own immune response.
NHS Blood and Transplant (NHSBT), which is collecting plasma for the study, said the latest research showed that men develop more coronavirus antibodies than women, making them better donors of plasma. Latest figures show that 43% of male donors had plasma rich enough in antibodies to be included in the trial, compared with 29% of female donors.
Professor David Roberts, associate director for blood donation at NHS Blood and Transplant, said: “We’d still like to hear from anybody who had coronavirus or the symptoms. More plasma donors are needed.
“But we’d especially want to hear from men. We test every plasma donation and men have higher antibody levels, which means we’re more likely to be able to use their plasma to save lives.
“Initially your immune system will try and fight off a virus with white blood cells. If you become more ill, your immune system needs to produce more antibodies that neutralize or kill the virus.
“Our studies, and many others around the world, show men with COVID-19 are more likely to become seriously ill than women. This makes them better plasma donors once they have recovered.”
It was confirmed last week that someone who has been tested positive for COVID-19 via the national testing program will be asked to participate in a blood plasma study. NHSBT said that people who have confirmed the virus through the ‘pillar 2’ national testing program will receive a text message 21 days after their results to see if they are interested in donating plasma. The texts will now be sent on a weekly basis to anyone who has been tested positive through the national testing program.
How does blood plasma help?
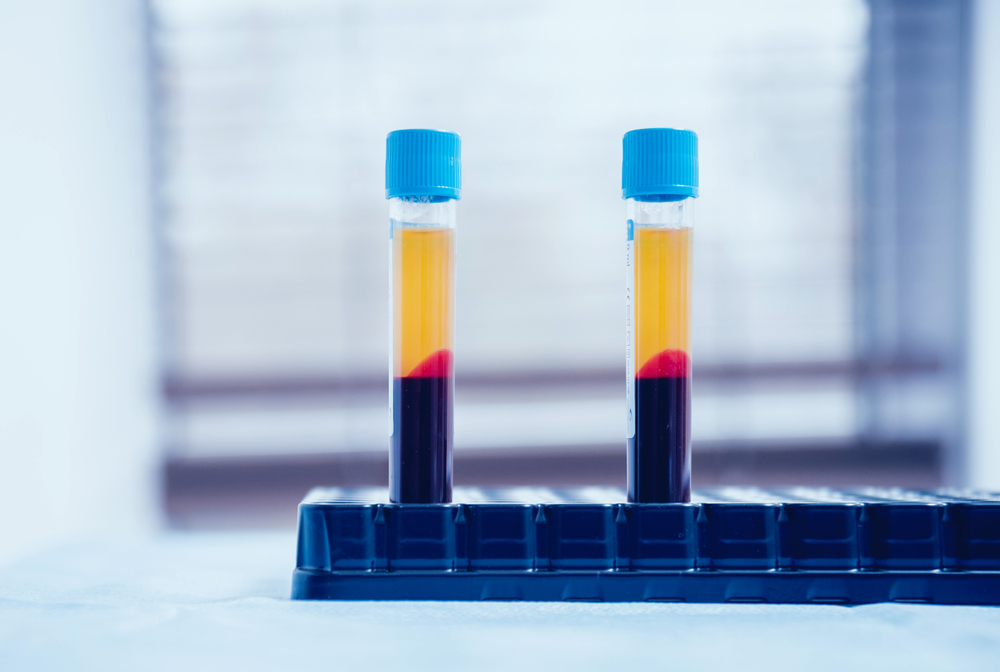
Plasma from former patients is rich in antibodies that develop as a person recovers from illness. This is transfused into people who are critically ill with COVID-19 and are unable to produce their own antibodies. If the trial is effective, the use of convalescent plasma could become a widespread practice in hospitals.
Two plasma donors presented their choice to donate as a “no-brainer.” Simon Callon, 51, of St Helens, Merseyside, survived COVID-19 but lost his father to Noel to the disease.
“I don’t want anybody going through what happened to my dad,” he said.
“He died on a hospital ward with no family or friends, with a nurse holding his hand. Only 10 people were allowed at his funeral.
“He’d had a fall at home but the paramedics found his oxygen levels were low and he had a high temperature so they took him in.
“He had been with my mum for more than 60 years. He was ex-RAF and a long-distance lorry driver but also an amateur painter who taught classes. His students formed a socially-distanced guard of honor with their paintbrushes.
“To me, donating plasma was a no-brainer. If you can save somebody or help somebody, you would do it.
“The donation was easy, no pain. The staff were brilliant. I hope I can help someone.”
Dr. Wassim Shamsuddin, an anesthetist specialist at the Milton Keynes University Hospital Foundation Trust, donated convalescent plasma to the Oxford Donor Centre after recovery from COVID-19.
The 40-year-old, from Bicester, said: “I have seen the effects of the virus first-hand and how it has taken the lives of many people, both old and young.
“When the opportunity came to donate plasma and hopefully antibodies to help others in the fight against COVID-19, it was a no-brainer for me.
“I have seen how the virus has disproportionately affected the BAME group, within the healthcare professionals and in the community.
“If plasma turns out to be one of the treatments shown to be of benefit to individuals then I would have played my part.”